Abstract
Purpose
Intracranial aneurysm (IA) rupture results in one of the most severe forms of stroke, with severe neurological sequelae. Inflammation appears to drive aneurysm formation and progression with macrophages playing a key role in this process. However, less is known about their involvement in aneurysm rupture. This study is aimed at demonstrating how relationship between the M1 (pro-inflammatory) and M2 (reparative) macrophage subtypes affect an aneurysm’s structure resulting in its rupture.
Methods
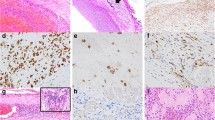
Forty-one saccular aneurysm wall samples were collected during surgery including 13 ruptured and 28 unruptured aneurysm sacs. Structural changes were evaluated using histological staining. Macrophages in the aneurysm wall were quantified and defined as M1 and M2 using HLA-DR and CD163 antibodies. Aneurysm samples were divided into four groups according to the structural changes and the M2/1 ratio. Data were analyzed using the Mann–Whitney U test.
Results
This study has demonstrated an association between the severity of structural changes of an aneurysm with inflammatory cell infiltration within its wall and subsequent aneurysm rupture. More severe morphological changes and a significantly higher number of inflammatory cells were observed in ruptured IAs (p < 0.001). There was a prevalence of M2 macrophage subtypes within the wall of ruptured aneurysms (p < 0.001). A subgroup of unruptured IAs with morphological and inflammatory changes similar to ruptured IAs was observed. The common feature of this subgroup was the presence of an intraluminal thrombus.
Conclusions
The degree of inflammatory cell infiltration associated with a shift in macrophage phenotype towards M2 macrophages could play an important role in structural changes of the aneurysm wall leading to its rupture.





Similar content being viewed by others
References
Aoki T, Frȍsen J, Fukuda M, Bando K, Shioi G, Tsuji K, Ollikainen E, Nozaki K, Laakkonen J, Narumiya S (2017) Prostaglandin E2–EP2–NF-κB signaling in macrophages as a potential therapeutic target for intracranial aneurysms. Sci Signal 10:eaah6037. https://doi.org/10.1126/scisignal.aah6037
Aoki T, Kataoka H, Ishibashi R, Nozaki K, Egashira K, Hashimoto N (2009) Impact of monocyte chemoattractant protein-1 deficiency on cerebral aneurysm formation. Stroke 40:942–951. https://doi.org/10.1161/STROKEAHA.108.532556
Aoki T, Kataoka H, Morimoto M, Nozaki K, Hashimoto N (2007) Macrophage-derived matrix metalloproteinase-2 and -9 promote the progression of cerebral aneurysms in rats. Stroke 38:162–169. https://doi.org/10.1161/01.STR.0000252129.18605.c8
Can A, Rudy RF, Castro VM, Yu S, Dligach D, Finan S, Gainer V, Shadick NA, Savova G, Murphy S, Cai T, Weiss ST, Du R (2018) Association between aspirin dose and subarachnoid hemorrhage from saccular aneurysms: a case-control study. Neurology 91:e1175–e1181. https://doi.org/10.1212/WNL.0000000000006200
Cebral J, Ollikainen E, Chung BJ, Mut F, Sippola V, Jahromi BR, Tulamo R, Hernesniemi J, Niemela M, Robertson A, Frosen J (2017) Flow conditions in the intracranial aneurysm lumen are associated with inflammation and degenerative changes of the aneurysm wall. AJNR Am J Neuroradiol 38:119–126. https://doi.org/10.3174/ajnr.A4951
Chalouhi N, Ali MS, Jabbour PM, Tjoumakaris SI, Gonzalez LF, Rosenwasser RH, Koch WJ, Dumont AS (2012) Biology of intracranial aneurysms: role of inflammation. J Cereb Blood Flow Metab 32:1659–1676. https://doi.org/10.1038/jcbfm.2012.84
Etminan N, Brown RD Jr, Beseoglu K, Juvela S, Raymond J, Morita A, Torner JC, Derdeyn CP, Raabe A, Mocco J, Korja M, Abdulazim A, Amin-Hanjani S, Al-Shahi Salman R, Barrow DL, Bederson J, Bonafe A, Dumont AS, Fiorella DJ, Gruber A, Hankey GJ, Hasan DM, Hoh BL, Jabbour P, Kasuya H, Kelly ME, Kirkpatrick PJ, Knuckey N, Koivisto T, Krings T, Lawton MT, Marotta TR, Mayer SA, Mee E, Pereira VM, Molyneux A, Morgan MK, Mori K, Murayama Y, Nagahiro S, Nakayama N, Niemela M, Ogilvy CS, Pierot L, Rabinstein AA, Roos YB, Rinne J, Rosenwasser RH, Ronkainen A, Schaller K, Seifert V, Solomon RA, Spears J, Steiger HJ, Vergouwen MD, Wanke I, Wermer MJ, Wong GK, Wong JH, Zipfel GJ, Connolly ES Jr, Steinmetz H, Lanzino G, Pasqualin A, Rufenacht D, Vajkoczy P, McDougall C, Hanggi D, LeRoux P, Rinkel GJ, Macdonald RL (2015) The unruptured intracranial aneurysm treatment score: a multidisciplinary consensus. Neurology 85:881–889. https://doi.org/10.1212/WNL.0000000000001891
Frosen J, Cebral J, Robertson AM, Aoki T (2019) Flow-induced, inflammation-mediated arterial wall remodeling in the formation and progression of intracranial aneurysms. Neurosurg Focus 47:E21. https://doi.org/10.3171/2019.5.FOCUS19234
Frösen J, Piippo A, Paetau A, Kangasniemi M, Niemelä M, Hernesniemi J, Jääskeläinen J (2004) Remodeling of saccular cerebral artery aneurysm wall is associated with rupture: histological analysis of 24 unruptured and 42 ruptured cases. Stroke 35:2287–2293. https://doi.org/10.1161/01.STR.0000140636.30204.da
Greving JP, Wermer MJ, Brown RD Jr, Morita A, Juvela S, Yonekura M, Ishibashi T, Torner JC, Nakayama T, Rinkel GJ, Algra A (2014) Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: a pooled analysis of six prospective cohort studies. Lancet Neurol 13:59–66. https://doi.org/10.1016/S1474-4422(13)70263-1
Hasan D, Chalouhi N, Jabbour P, Hashimoto T (2012) Macrophage imbalance (M1 vs. M2) and upregulation of mast cells in wall of ruptured human cerebral aneurysms: preliminary results. J Neuroinflammation 9:222. https://doi.org/10.1186/1742-2094-9-222
Hasan D, Hashimoto T, Kung D, Macdonald RL, Winn HR, Heistad D (2012) Upregulation of cyclooxygenase-2 (COX-2) and microsomal prostaglandin E2 synthase-1 (mPGES-1) in wall of ruptured human cerebral aneurysms: preliminary results. Stroke 43:1964–1967. https://doi.org/10.1161/STROKEAHA.112.655829
Hasan DM, Chalouhi N, Jabbour P, Dumont AS, Kung DK, Magnotta VA, Young WL, Hashimoto T, Richard Winn H, Heistad D (2013) Evidence that acetylsalicylic acid attenuates inflammation in the walls of human cerebral aneurysms: preliminary results. J Am Heart Assoc 2:e000019. https://doi.org/10.1161/JAHA.112.000019
Hosaka K, Hoh BL (2014) Inflammation and cerebral aneurysms. Transl Stroke Res 5:190–198. https://doi.org/10.1007/s12975-013-0313-y
Ishibashi T, Murayama Y, Urashima M, Saguchi T, Ebara M, Arakawa H, Irie K, Takao H, Abe T (2009) Unruptured intracranial aneurysms: incidence of rupture and risk factors. Stroke 40:313–316. https://doi.org/10.1161/strokeaha.108.521674
Jayaraman T, Berenstein V, Li X, Mayer J, Silane M, Shin YS, Niimi Y, Kilic T, Gunel M, Berenstein A (2005) Tumor necrosis factor alpha is a key modulator of inflammation in cerebral aneurysms. Neurosurgery 57:558–564. https://doi.org/10.1227/01.neu.0000170439.89041.d6
Juvela S, Poussa K, Lehto H, Porras M (2013) Natural history of unruptured intracranial aneurysms. Stroke 44:2414–2421. https://doi.org/10.1161/strokeaha.113.001838
Kanematsu Y, Kanematsu M, Kurihara C, Tada Y, Tsou TL, van Rooijen N, Lawton MT, Young WL, Liang EI, Nuki Y, Hashimoto T (2011) Critical roles of macrophages in the formation of intracranial aneurysm. Stroke 42:173–178. https://doi.org/10.1161/STROKEAHA.110.590976
Kataoka K, Taneda M, Asai T, Kinoshita A, Ito M, Kuroda R (1999) Structural fragility and inflammatory response of ruptured cerebral aneurysms. A comparative study between ruptured and unruptured cerebral aneurysms. Stroke 30:1396–1401. https://doi.org/10.1161/01.str.30.7.1396
Ke X, Chen C, Song Y, Cai Q, Li J, Tang Y, Han X, Qu W, Chen A, Wang H, Xu G, Liu D (2019) Hypoxia modifies the polarization of macrophages and their inflammatory microenvironment, and inhibits malignant behavior in cancer cells. Oncol Lett. https://doi.org/10.3892/ol.2019.10956
Krings T, Mandell DM, Kiehl TR, Geibprasert S, Tymianski M, Alvarez H, terBrugge KG, Hans FJ (2011) Intracranial aneurysms: from vessel wall pathology to therapeutic approach. Nat Rev Neurol 7:547–559. https://doi.org/10.1038/nrneurol.2011.136
Kurki MI, Häkkinen SK, Frösen J, Tulamo R, von und zu Fraunberg M, Wong G, Tromp G, Niemelä M, Hernesniemi J, Jääskeläinen JE, Ylä-Herttuala S (2011) Upregulated signaling pathways in ruptured human saccular intracranial aneurysm wall: an emerging regulative role of Toll-like receptor signaling and nuclear factor-κB, hypoxia-inducible factor-1A, and ETS transcription factors. Neurosurgery 68:1667–1675. https://doi.org/10.1227/NEU.0b013e318210f001 (discussion 1675-1666)
Laaksamo E, Tulamo R, Liiman A, Baumann M, Friedlander RM, Hernesniemi J, Kangasniemi M, Niemelä M, Laakso A, Frösen J (2013) Oxidative stress is associated with cell death, wall degradation, and increased risk of rupture of the intracranial aneurysm wall. Neurosurgery 72:109–117. https://doi.org/10.1227/NEU.0b013e3182770e8c
Macdonald RL, Schweizer TA (2017) Spontaneous subarachnoid haemorrhage. The Lancet 389:655–666. https://doi.org/10.1016/s0140-6736(16)30668-7
Mantovani A, Sozzani S, Locati M, Allavena P, Sica A (2002) Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol 23:549–555. https://doi.org/10.1016/s1471-4906(02)02302-5
Martin-Ventura JL, Madrigal-Matute J, Martinez-Pinna R, Ramos-Mozo P, Blanco-Colio LM, Moreno JA, Tarin C, Burillo E, Fernandez-Garcia CE, Egido J, Meilhac O, Michel JB (2012) Erythrocytes, leukocytes and platelets as a source of oxidative stress in chronic vascular diseases: detoxifying mechanisms and potential therapeutic options. Thromb Haemost 108:435–442. https://doi.org/10.1160/th12-04-0248
Martinez-Pinna R, Ramos-Mozo P, Madrigal-Matute J, Blanco-Colio LM, Lopez JA, Calvo E, Camafeita E, Lindholt JS, Meilhac O, Delbosc S, Michel JB, Vega de Ceniga M, Egido J, Martin-Ventura JL (2011) Identification of peroxiredoxin-1 as a novel biomarker of abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol 31:935–943. https://doi.org/10.1161/atvbaha.110.214429
Meng H, Tutino VM, Xiang J, Siddiqui A (2014) High WSS or Low WSS? Complex interactions of hemodynamics with intracranial aneurysm initiation, growth, and rupture: toward a unifying hypothesis. Am J Neuroradiol 35:1254–1262. https://doi.org/10.3174/ajnr.a3558
Nieuwkamp DJ, Setz LE, Algra A, Linn FH, De Rooij NK, Rinkel GJ (2009) Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol 8:635–642. https://doi.org/10.1016/s1474-4422(09)70126-7
Nowicki KW, Hosaka K, Walch FJ, Scott EW, Hoh BL (2018) M1 macrophages are required for murine cerebral aneurysm formation. J Neurointerv Surg 10:93–97. https://doi.org/10.1136/neurintsurg-2016-012911
Ollikainen E, Tulamo R, Frosen J, Lehti S, Honkanen P, Hernesniemi J, Niemela M, Kovanen PT (2014) Mast cells, neovascularization, and microhemorrhages are associated with saccular intracranial artery aneurysm wall remodeling. J Neuropathol Exp Neurol 73:855–864. https://doi.org/10.1097/NEN.0000000000000105
Ollikainen E, Tulamo R, Kaitainen S, Honkanen P, Lehti S, Liimatainen T, Hernesniemi J, Niemela M, Kovanen PT, Frosen J (2018) Macrophage infiltration in the saccular intracranial aneurysm wall as a response to locally lysed erythrocytes that promote degeneration. J Neuropathol Exp Neurol 77:890–903. https://doi.org/10.1093/jnen/nly068
Signorelli F, Sela S, Gesualdo L, Chevrel S, Tollet F, Pailler-Mattei C, Tacconi L, Turjman F, Vacca A, Schul DB (2018) Hemodynamic stress, inflammation, and intracranial aneurysm development and rupture: a systematic review. World Neurosurg 115:234–244. https://doi.org/10.1016/j.wneu.2018.04.143
Tulamo R, Frosen J, Hernesniemi J, Niemela M (2018) Inflammatory changes in the aneurysm wall: a review. J Neurointerv Surg 10:i58–i67. https://doi.org/10.1136/jnis.2009.002055.rep
Tulamo R, Frösen J, Junnikkala S, Paetau A, Pitkäniemi J, Kangasniemi M, Niemelä M, Jääskeläinen J, Jokitalo E, Karatas A, Hernesniemi J, Meri S (2006) Complement activation associates with saccular cerebral artery aneurysm wall degeneration and rupture. Neurosurgery 59:1069–1076. https://doi.org/10.1227/01.Neu.0000245598.84698.26 (discussion 1076-1067)
Van Gijn J, Kerr RS, Rinkel GJ (2007) Subarachnoid haemorrhage. The Lancet 369:306–318. https://doi.org/10.1016/s0140-6736(07)60153-6
Vlak MH, Algra A, Brandenburg R, Rinkel GJ (2011) Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol 10:626–636. https://doi.org/10.1016/s1474-4422(11)70109-0
Vorp DA, Lee PC, Wang DHJ, Makaroun MS, Nemoto EM, Ogawa S, Webster MW (2001) Association of intraluminal thrombus in abdominal aortic aneurysm with local hypoxia and wall weakening. J Vasc Surg 34:291–299. https://doi.org/10.1067/mva.2001.114813
Yamashiro S, Uchikawa H, Yoshikawa M, Kuriwaki K, Hitoshi Y, Yoshida A, Komohara Y, Mukasa A (2019) Histological analysis of infiltrating macrophages in the cerebral aneurysm walls. J Clin Neurosci 67:204–209. https://doi.org/10.1016/j.jocn.2019.05.027
Zanaty M, Roa JA, Nakagawa D, Chalouhi N, Allan L, Al Kasab S, Limaye K, Ishii D, Samaniego EA, Jabbour P, Torner JC, Hasan DM (2019) Aspirin associated with decreased rate of intracranial aneurysm growth. J Neurosurg 1–8. https://doi.org/10.3171/2019.6.jns191273
Acknowledgements
We would like to acknowledge Dr. Jan Lodin, a native speaker, for his assistance in proofreading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The approval of the Ethics Committee of Masaryk Hospital, Ústí nad Labem (Reference Number: 238/59), was obtained on 22 June 2016.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery - Aneurysm
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stratilová, M.H., Koblížek, M., Štekláčová, A. et al. Increased macrophage M2/M1 ratio is associated with intracranial aneurysm rupture. Acta Neurochir 165, 177–186 (2023). https://doi.org/10.1007/s00701-022-05418-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05418-0