Abstract
Polymers are omnipresent materials that are widely used in medicine, e.g., as construction materials for medical devices or as polymer nanoparticle drug delivery systems. Therefore, their possible effects on biomolecules, such as lipids, proteins, and other molecules, present in the human body must be examined. This review addresses the effects of polymer materials (such as dendrimers, polysaccharides) on the process of amyloid fibril formation. Amyloidoses are very serious diseases that are characterized by amyloid deposition in various organs and tissues, causing their dysfunction. The treatment of amyloidoses, such as Alzheimer’s disease (AD), using polymer materials is a challenge. Studies aiming to elucidate the effects of polymers on the process of amyloid fibril formation are therefore also of key importance for understanding the process of amyloid fibril formation and amyloidoses in general.

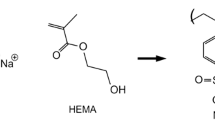
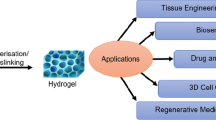
Graphical abstract

















Similar content being viewed by others
References
Chuang E, Hori AM, Hesketh CD, Shorter J (2018) Amyloid assembly and disassembly. J Cell Sci 131:jcs189928. https://doi.org/10.1242/jcs.189928
Radford SE, Weissman JS (2012) Special issue: the molecular and cellular mechanisms of amyloidosis. J Mol Biol 421:139–141. https://doi.org/10.1016/j.jmb.2012.05.042
Sideras K, Gertz MA (2009) Chapter 1 amyloidosis. In: Advances in clinical chemistry. pp 1–44
Sipe JD, Benson MD, Buxbaum JN, Ikeda SI, Merlini G, Saraiva MJM, Westermark P (2010) Amyloid fibril protein nomenclature: 2010 recommendations from the nomenclature committee of the International Society of Amyloidosis. Amyloid 17:101–104. https://doi.org/10.3109/13506129.2010.526812
Serpell LC, Sunde M, Benson MD, Tennent GA, Pepys MB, Fraser PE (2000) The protofilament substructure of amyloid fibrils. J Mol Biol 300:1033–1039. https://doi.org/10.1006/jmbi.2000.3908
Ionescu-Zanetti C, Khurana R, Gillespie JR, Petrick JS, Trabachino LC, Minert LJ, Carter SA, Fink AL (1999) Monitoring the assembly of Ig light-chain amyloid fibrils by atomic force microscopy. Proc Natl Acad Sci 96:13175–13179. https://doi.org/10.1073/pnas.96.23.13175
Taglialegna A, Lasa I, Valle J (2016) Amyloid structures as biofilm matrix scaffolds. J Bacteriol 198:2579–2588. https://doi.org/10.1128/JB.00122-16
Holubová M, Hrubý M (2016) Terapeutika amyloidóz. Chem List 110:851–859
Wei G, Su Z, Reynolds NP, Arosio P, Hamley IW, Gazit E, Mezzenga R (2017) Self-assembling peptide and protein amyloids: from structure to tailored function in nanotechnology. Chem Soc Rev 46:4661–4708. https://doi.org/10.1039/C6CS00542J
Cheung H-Y, Lau K-T, Ho M-P, Mosallam A (2009) Study on the mechanical properties of different silkworm silk fibers. J Compos Mater 43:2521–2531. https://doi.org/10.1177/0021998309345347
Engineering ToolBox (2003) Young’s modulus - tensile and yield strength for common materials. https://www.engineeringtoolbox.com/young-modulus-d_417.html. Accessed 27 Feb 2020
Hori Y, Hashimoto T, Nomoto H, Hyman BT, Iwatsubo T (2015) Role of apolipoprotein E in β-amyloidogenesis: isoform-specific effects on protofibril to fibril conversion of Aβ in vitro and brain Aβ deposition in vivo. J Biol Chem 290:15163–15174. https://doi.org/10.1074/jbc.M114.622209
Bemporad F, Chiti F (2013) Pathways of amyloid formation. Amyloid fibrils and prefibrillar aggregates. Wiley-VCH Verlag GmbH & Co. KGaA, Weinheim, pp 151–166
Arosio P, Knowles TPJ, Linse S (2015) On the lag phase in amyloid fibril formation. Phys Chem Chem Phys 17:7606–7618. https://doi.org/10.1039/c4cp05563b
Iannuzzi C, Maritato R, Irace G, Sirangelo I (2013) Misfolding and amyloid aggregation of apomyoglobin. Int J Mol Sci 14:14287–14300. https://doi.org/10.3390/ijms140714287
Hurshman AR, White JT, Powers ET, Kelly JW (2004) Transthyretin aggregation under partially denaturing conditions is a downhill polymerization. Biochemistry 43:7365–7381. https://doi.org/10.1021/bi049621l
Gazit E (2005) Mechanisms of amyloid fibril self-assembly and inhibition. FEBS J 272:5971–5978. https://doi.org/10.1111/j.1742-4658.2005.05022.x
Marshall KE, Morris KL, Charlton D, O’Reilly N, Lewis L, Walden H, Serpell LC (2011) Hydrophobic, aromatic, and electrostatic interactions play a central role in amyloid fibril formation and stability. Biochemistry 50:2061–2071. https://doi.org/10.1021/bi101936c
Chiti F, Dobson CM (2006) Protein misfolding, functional amyloid, and human disease. Annu Rev Biochem 75:333–366. https://doi.org/10.1146/annurev.biochem.75.101304.123901
Mülhaupt R (2004) Hermann Staudinger and the origin of macromolecular chemistry. Angew Chem Int Ed 43:1054–1063. https://doi.org/10.1002/anie.200330070
Nimesh S (2013) Dendrimers. In: Gene therapy. Elsevier, pp 259–285
Abbasi E, Aval SF, Akbarzadeh A et al (2014) Dendrimers: synthesis, applications, and properties. Nanoscale Res Lett 9:1–10
Noriega-Luna B, Godínez LA, Rodríguez FJ, Rodríguez A, Zaldívar-Lelo de Larrea G, Sosa-Ferreyra CF, Mercado-Curiel RF, Manríquez J, Bustos E (2014) Applications of dendrimers in drug delivery agents, diagnosis, therapy, and detection. J Nanomater 2014:1–19. https://doi.org/10.1155/2014/507273
Klajnert B, Stanisławska L, Bryszewska M, Pałecz B (2003) Interactions between PAMAM dendrimers and bovine serum albumin. Biochim Biophys Acta, Proteins Proteomics 1648:115–126. https://doi.org/10.1016/S1570-9639(03)00117-1
Klajnert B, Cortijo-Arellano M, Cladera J, Bryszewska M (2006) Influence of dendrimer’s structure on its activity against amyloid fibril formation. Biochem Biophys Res Commun 345:21–28. https://doi.org/10.1016/j.bbrc.2006.04.041
Klajnert B, Cortijo-Arellano M, Bryszewska M, Cladera J (2006) Influence of heparin and dendrimers on the aggregation of two amyloid peptides related to Alzheimer’s and prion diseases. Biochem Biophys Res Commun 339:577–582. https://doi.org/10.1016/j.bbrc.2005.11.053
Sengupta U, Nilson AN, Kayed R (2016) The role of amyloid-β oligomers in toxicity, propagation, and immunotherapy. EBioMedicine 6:42–49. https://doi.org/10.1016/j.ebiom.2016.03.035
Rekas A, Lo V, Gadd GE, Cappai R, Yun SI (2009) PAMAM dendrimers as potential agents against fibrillation of α-synuclein, a Parkinson’s disease-related protein. Macromol Biosci 9:230–238. https://doi.org/10.1002/mabi.200800242
Inoue M, Ueda M, Higashi T, Anno T, Fujisawa K, Motoyama K, Mizuguchi M, Ando Y, Jono H, Arima H (2019) Therapeutic potential of polyamidoamine dendrimer for amyloidogenic transthyretin amyloidosis. ACS Chem Neurosci 10:2584–2590. https://doi.org/10.1021/acschemneuro.9b00059
Gurzov EN, Wang B, Pilkington EH, Chen P, Kakinen A, Stanley WJ, Litwak SA, Hanssen EG, Davis TP, Ding F, Ke PC (2016) Inhibition of hIAPP amyloid aggregation and pancreatic β-cell toxicity by OH-terminated PAMAM dendrimer. Small 12:1615–1626. https://doi.org/10.1002/smll.201502317
Heegaard PMH, Pedersen HG, Flink J, Boas U (2004) Amyloid aggregates of the prion peptide PrP106-126 are destabilised by oxidation and by the action of dendrimers. FEBS Lett 577:127–133. https://doi.org/10.1016/j.febslet.2004.09.073
Supattapone S, Wille H, Uyechi L, Safar J, Tremblay P, Szoka FC, Cohen FE, Prusiner SB, Scott MR (2001) Branched polyamines cure prion-infected neuroblastoma cells. J Virol 75:3453–3461. https://doi.org/10.1128/jvi.75.7.3453-3461.2001
Klementieva O, Benseny-Cases N, Gella A, Appelhans D, Voit B, Cladera J (2011) Dense shell glycodendrimers as potential nontoxic anti-amyloidogenic agents in Alzheimer’s disease. Amyloid–dendrimer aggregates morphology and cell toxicity. Biomacromolecules 12:3903–3909. https://doi.org/10.1021/bm2008636
Klementieva O, Aso E, Filippini D, Benseny-Cases N, Carmona M, Juvés S, Appelhans D, Cladera J, Ferrer I (2013) Effect of poly(propylene imine) glycodendrimers on β-amyloid aggregation in vitro and in APP/PS1 transgenic mice, as a model of brain amyloid deposition and Alzheimer’s disease. Biomacromolecules 14:3570–3580. https://doi.org/10.1021/bm400948z
Aso E, Martinsson I, Appelhans D, Effenberg C, Benseny-Cases N, Cladera J, Gouras G, Ferrer I, Klementieva O (2019) Poly(propylene imine) dendrimers with histidine-maltose shell as novel type of nanoparticles for synapse and memory protection. Nanomed Nanotechnol Biol Med 17:198–209. https://doi.org/10.1016/j.nano.2019.01.010
Laumann K, Boas U, Larsen HM, Heegaard PMH, Bergström AL (2015) Urea and thiourea modified polypropyleneimine dendrimers clear intracellular α-synuclein aggregates in a human cell line. Biomacromolecules 16:116–124. https://doi.org/10.1021/bm501244m
McCarthy JM, Rasines Moreno B, Filippini D et al (2013) Influence of surface groups on poly(propylene imine) dendrimers antiprion activity. Biomacromolecules 14:27–37. https://doi.org/10.1021/bm301165u
Sorokina SA, Stroylova YY, Tishina SA, Shifrina ZB, Muronetz VI (2019) Promising anti-amyloid behavior of cationic pyridylphenylene dendrimers: role of structural features and mechanism of action. Eur Polym J 116:20–29. https://doi.org/10.1016/j.eurpolymj.2019.03.053
Popova E, Khamidova D, Neelov I, Komilov F (2018) Lysine dendrimers and their complexes with therapeutic and amyloid peptides: computer simulation. In: Dendrimers - fundamentals and applications. InTech
Sorokina SA, Stroylova YY, Shifrina ZB, Muronetz VI (2016) Disruption of amyloid prion protein aggregates by cationic pyridylphenylene dendrimers. Macromol Biosci 16:266–275. https://doi.org/10.1002/mabi.201500268
Milowska K, Szwed A, Mutrynowska M, Gomez-Ramirez R, de la Mata FJ, Gabryelak T, Bryszewska M (2015) Carbosilane dendrimers inhibit α-synuclein fibrillation and prevent cells from rotenone-induced damage. Int J Pharm 484:268–275. https://doi.org/10.1016/j.ijpharm.2015.02.066
Cannon JR, Tapias V, Na HM, Honick AS, Drolet RE, Greenamyre JT (2009) A highly reproducible rotenone model of Parkinson’s disease. Neurobiol Dis 34:279–290. https://doi.org/10.1016/j.nbd.2009.01.016
Milowska K, Grochowina J, Katir N, el Kadib A, Majoral JP, Bryszewska M, Gabryelak T (2013) Viologen-phosphorus dendrimers inhibit α-synuclein fibrillation. Mol Pharm 10:1131–1137. https://doi.org/10.1021/mp300636h
Milowska K, Gabryelak T, Bryszewska M, Caminade AM, Majoral JP (2012) Phosphorus-containing dendrimers against α-synuclein fibril formation. Int J Biol Macromol 50:1138–1143. https://doi.org/10.1016/j.ijbiomac.2012.02.003
Nguyen PT, Sharma R, Rej R, de Carufel CA, Roy R, Bourgault S (2016) Low generation anionic dendrimers modulate islet amyloid polypeptide self-assembly and inhibit pancreatic β-cell toxicity. RSC Adv 6:76360–76369. https://doi.org/10.1039/c6ra15373a
Baldrighi M, Trusel M, Tonini R, Giordani S (2016) Carbon nanomaterials interfacing with neurons: an in vivo perspective. Front Neurosci 10:250
Chertok B, Moffat BA, David AE, Yu F, Bergemann C, Ross BD, Yang VC (2008) Iron oxide nanoparticles as a drug delivery vehicle for MRI monitored magnetic targeting of brain tumors. Biomaterials 29:487–496. https://doi.org/10.1016/j.biomaterials.2007.08.050
Wang M, Kakinen A, Pilkington EH, Davis TP, Ke PC (2017) Differential effects of silver and iron oxide nanoparticles on IAPP amyloid aggregation. Biomater Sci 5:485–493. https://doi.org/10.1039/C6BM00764C
Palmal S, Jana NR, Jana NR (2014) Inhibition of amyloid fibril growth by nanoparticle coated with histidine-based polymer. J Phys Chem C 118:21630–21638. https://doi.org/10.1021/jp505613g
Bobylev AG, Shpagina MD, Bobyleva LG, Okuneva AD, Piotrovsky LB, Podlubnaya ZA (2012) Antiamyloid properties of fullerene C60 derivatives. Biophysics (Oxf) 57:300–304. https://doi.org/10.1134/S0006350912030050
Bobylev AG, Marsagishvili LG, Podlubnaya ZA (2010) Fluorescence analysis of the action of soluble derivatives of fullerene C60 on amyloid fibrils of the brain peptide Aβ(1–42). Biophysics (Oxf) 55:699–702. https://doi.org/10.1134/S0006350910050027
Marsagishvili LG, Bobylev AG, Shpagina MD, Troshin PA, Podlubnaya ZA (2009) Effect of fullerenes C60 on X-protein amyloids. Biophysics (Oxf) 54:135–138. https://doi.org/10.1134/S000635090902002X
Wei D, Qian W (2008) Facile synthesis of Ag and Au nanoparticles utilizing chitosan as a mediator agent. Colloids Surf B: Biointerfaces 62:136–142. https://doi.org/10.1016/j.colsurfb.2007.09.030
Sen S, Konar S, Das B, Pathak A, Dhara S, Dasgupta S, DasGupta S (2016) Inhibition of fibrillation of human serum albumin through interaction with chitosan-based biocompatible silver nanoparticles. RSC Adv 6:43104–43115. https://doi.org/10.1039/c6ra05129d
McLaurin J, Franklin T, Zhang X, Deng J, Fraser PE (1999) Interactions of Alzheimer amyloid-β peptides with glycosaminoglycans. Eur J Biochem 266:1101–1110. https://doi.org/10.1046/j.1432-1327.1999.00957.x
Cohlberg JA, Li J, Uversky VN, Fink AL (2002) Heparin and other glycosaminoglycans stimulate the formation of amyloid fibrils from α-synuclein in vitro. Biochemistry 41:1502–1511. https://doi.org/10.1021/bi011711s
Stewart KL, Radford SE (2017) Amyloid plaques beyond Aβ: a survey of the diverse modulators of amyloid aggregation. Biophys Rev 9:405–419. https://doi.org/10.1007/s12551-017-0271-9
Dı́az-Nido J, Wandosell F, Avila J (2002) Glycosaminoglycans and β-amyloid, prion and tau peptides in neurodegenerative diseases. Peptides 23:1323–1332. https://doi.org/10.1016/S0196-9781(02)00068-2
Magnus JH, Stenstad T (1997) Proteoglycans and the extracellular matrix in amyloidosis. Amyloid 4:121–134. https://doi.org/10.3109/13506129708995282
Valle-Delgado JJ, Alfonso-Prieto M, Groot NS, Ventura S, Samitier J, Rovira C, Fernàndez-Busquets X (2010) Modulation of Aβ 42 fìbrillogenesis by glycosaminoglycan structure. FASEB J 24:4250–4261. https://doi.org/10.1096/fj.09-153551
Radko SP, Khmeleva SA, Mantsyzov AB, Kiseleva YY, Mitkevich VA, Kozin SA, Makarov AA (2018) Heparin modulates the kinetics of zinc-induced aggregation of amyloid-β peptides. J Alzheimers Dis 63:539–550. https://doi.org/10.3233/JAD-171120
Caughey B, Raymond GJ (1993) Sulfated polyanion inhibition of scrapie-associated PrP accumulation in cultured cells. J Virol 67:643–650. https://doi.org/10.1128/JVI.67.2.643-650.1993
Rosú SA, Toledo L, Urbano BF, Sanchez SA, Calabrese GC, Tricerri MA (2017) Learning from synthetic models of extracellular matrix; differential binding of wild type and amyloidogenic human apolipoprotein A-I to hydrogels formed from molecules having charges similar to those found in natural GAGs. Protein J 36:374–383. https://doi.org/10.1007/s10930-017-9728-8
Castellani R, Siedlak S, Fortino A, Perry G, Ghetti B, Smith M (2005) Chitin-like polysaccharides in Alzheimers disease brains. Curr Alzheimer Res 2:419–423. https://doi.org/10.2174/156720505774330555
Castellani RJ, Perry G, Smith MA (2007) The role of novel chitin-like polysaccharides in Alzheimer disease. Neurotox Res 12:269–274. https://doi.org/10.1007/BF03033910
Sotgiu S, Musumeci S, Marconi S, Gini B, Bonetti B (2008) Different content of chitin-like polysaccharides in multiple sclerosis and Alzheimer’s disease brains. J Neuroimmunol 197:70–73. https://doi.org/10.1016/j.jneuroim.2008.03.021
Semenyuk P, Kurochkina L, Barinova K, Muronetz V (2020) Alpha-synuclein amyloid aggregation is inhibited by sulfated aromatic polymers and pyridinium polycation. Polymers (Basel) 12:517. https://doi.org/10.3390/polym12030517
Liu H, Ojha B, Morris C, Jiang M, Wojcikiewicz EP, Rao PPN, du D (2015) Positively charged chitosan and N-trimethyl chitosan inhibit Aβ40 fibrillogenesis. Biomacromolecules 16:2363–2373. https://doi.org/10.1021/acs.biomac.5b00603
Liu C, Zhang Y (2011) Nucleic acid-mediated protein aggregation and assembly. In: Advances in protein chemistry and structural biology. Academic Press Inc., pp 1–40
Calamai M, Kumita JR, Mifsud J, Parrini C, Ramazzotti M, Ramponi G, Taddei N, Chiti F, Dobson CM (2006) Nature and significance of the interactions between amyloid fibrils and biological polyelectrolytes. Biochemistry 45:12806–12815. https://doi.org/10.1021/bi0610653
Silva JL, Cordeiro Y (2016) The “Jekyll and Hyde” actions of nucleic acids on the prion-like aggregation of proteins. J Biol Chem 291:15482–15490
Mambule C, Ando Y, Anan I, Holmgren G, Sandgren O, Stigbrandt T, Tashima K, Suhr OB (2000) Enhancement of AA-amyloid formation in mice by transthyretin amyloid fragments and polyethylene glycol. Biochim Biophys Acta, Gen Subj 1474:331–336. https://doi.org/10.1016/S0304-4165(00)00032-5
Kotormán M, Simon L, Borics A, Szabó M, Szabó K, Szögi T, Fülöp L (2015) Amyloid-like fibril formation by trypsin in aqueous ethanol. Inhibition of fibrillation by PEG. Protein Pept Lett 22:1104–1110. https://doi.org/10.2174/0929866522666151002154324
Funtan S, Evgrafova Z, Adler J, Huster D, Binder W (2016) Amyloid beta aggregation in the presence of temperature-sensitive polymers. Polymers (Basel) 8:178. https://doi.org/10.3390/polym8050178
Nielsen L, Khurana R, Coats A, Frokjaer S, Brange J, Vyas S, Uversky VN, Fink AL (2001) Effect of environmental factors on the kinetics of insulin fibril formation: elucidation of the molecular mechanism. Biochemistry 40:6036–6046. https://doi.org/10.1021/bi002555c
Wallin C, Friedemann M, Sholts SB, Noormägi A, Svantesson T, Jarvet J, Roos PM, Palumaa P, Gräslund A, Wärmländer SKTS (2020) Mercury and Alzheimer’s disease: Hg(II) ions display specific binding to the amyloid-β peptide and hinder its fibrillization. Biomolecules 10:44. https://doi.org/10.3390/biom10010044
Evstafyeva DB, Izumrudov VA, Muronetz VI, Semenyuk PI (2018) Tightly bound polyelectrolytes enhance enzyme proteolysis and destroy amyloid aggregates. Soft Matter 14:3768–3773. https://doi.org/10.1039/c8sm00101d
Assarsson A, Linse S, Cabaleiro-Lago C (2014) Effects of polyamino acids and polyelectrolytes on amyloid β fibril formation. Langmuir 30:8812–8818. https://doi.org/10.1021/la501414j
Cabaleiro-Lago C, Quinlan-Pluck F, Lynch I, Lindman S, Minogue AM, Thulin E, Walsh DM, Dawson KA, Linse S (2008) Inhibition of amyloid β protein fibrillation by polymeric nanoparticles. J Am Chem Soc 130:15437–15443. https://doi.org/10.1021/ja8041806
Jiang Z, Dong X, Sun Y (2018) Charge effects of self-assembled chitosan-hyaluronic acid nanoparticles on inhibiting amyloid β-protein aggregation. Carbohydr Res 461:11–18. https://doi.org/10.1016/j.carres.2018.03.001
Baysal I, Yabanoglu-Ciftci S, Tunc-Sarisozen Y, Ulubayram K, Ucar G (2013) Interaction of selegiline-loaded PLGA-b-PEG nanoparticles with beta-amyloid fibrils. J Neural Transm 120:903–910. https://doi.org/10.1007/s00702-013-0992-2
Baysal I, Ucar G, Gultekinoglu M, Ulubayram K, Yabanoglu-Ciftci S (2017) Donepezil loaded PLGA-b-PEG nanoparticles: their ability to induce destabilization of amyloid fibrils and to cross blood brain barrier in vitro. J Neural Transm 124:33–45. https://doi.org/10.1007/s00702-016-1527-4
Birks J, Flicker L (2003) Selegiline for Alzheimer’s disease. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd000442
Giorgetti S, Greco C, Tortora P, Aprile FA (2018) Targeting amyloid aggregation: an overview of strategies and mechanisms. Int J Mol Sci 19
Gazit E (2002) A possible role for π-stacking in the self-assembly of amyloid fibrils. FASEB J 16:77–83. https://doi.org/10.1096/fj.01-0442hyp
Findeis MA, Musso GM, Arico-Muendel CC, Benjamin HW, Hundal AM, Lee JJ, Chin J, Kelley M, Wakefield J, Hayward NJ, Molineaux SM (1999) Modified-peptide inhibitors of amyloid β-peptide polymerization. Biochemistry 38:6791–6800. https://doi.org/10.1021/bi982824n
Soto C, Sigurdsson EM, Morelli L, Asok Kumar R, Castaño EM, Frangione B (1998) β-Sheet breaker peptides inhibit fibrillogenesis in a rat brain model of amyloidosis: implications for Alzheimer’s therapy. Nat Med 4:822–826. https://doi.org/10.1038/nm0798-822
Tjernberg LO, Näslundt J, Lindqvist F et al (1996) Arrest of β-amyloid fibril formation by a pentapeptide ligand. J Biol Chem 271:8545–8548. https://doi.org/10.1074/jbc.271.15.8545
Porat Y, Abramowitz A, Gazit E (2006) Inhibition of amyloid fibril formation by polyphenols: structural similarity and aromatic interactions as a common inhibition mechanism. Chem Biol Drug Des 67:27–37. https://doi.org/10.1111/j.1747-0285.2005.00318.x
Vilcacundo R, Méndez P, Reyes W, Romero H, Pinto A, Carrillo W (2018) Antibacterial activity of hen egg white lysozyme denatured by thermal and chemical treatments. Sci Pharm 86:48. https://doi.org/10.3390/scipharm86040048
Jiang D, Rauda I, Han S, Chen S, Zhou F (2012) Aggregation pathways of the amyloid β(1 42) peptide depend on its colloidal stability and ordered β-sheet stacking. Langmuir 28:12711–12721. https://doi.org/10.1021/la3021436
Hortschansky P, Schroeckh V, Christopeit T, Zandomeneghi G, Fändrich M (2005) The aggregation kinetics of Alzheimer’s β-amyloid peptide is controlled by stochastic nucleation. Protein Sci 14:1753–1759. https://doi.org/10.1110/ps.041266605
Liu P, Zhang S, Chen MS, Liu Q, Wang C, Wang C, Li YM, Besenbacher F, Dong M (2012) Co-assembly of human islet amyloid polypeptide (hIAPP)/insulin. Chem Commun 48:191–193. https://doi.org/10.1039/c1cc14285b
Holubova M, Konefał R, Moravkova Z, Zhigunov A, Svoboda J, Pop-Georgievski O, Hromadkova J, Groborz O, Stepanek P, Hruby M (2017) Carbon nanospecies affecting amyloid formation. RSC Adv 7:53887–53898. https://doi.org/10.1039/C7RA11296C
Hirsh SL, McKenzie DR, Nosworthy NJ et al (2013) The Vroman effect: competitive protein exchange with dynamic multilayer protein aggregates. Colloids Surf B: Biointerfaces 103:395–404. https://doi.org/10.1016/j.colsurfb.2012.10.039
Funding
Monika Holubová received financial support from Charles University, project GA UK No. 386218. PS and MH also received financial support from the Czech Science Foundation (grants nos. 19-01438S and 18-07983S).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Holubová, M., Štěpánek, P. & Hrubý, M. Polymer materials as promoters/inhibitors of amyloid fibril formation. Colloid Polym Sci 299, 343–362 (2021). https://doi.org/10.1007/s00396-020-04710-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00396-020-04710-8