Abstract
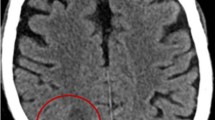
Cerebral abscesses caused by dark-pigmented Fonsecaea fungi are rare, especially in otherwise healthy individuals. In this case report, we present a 61-year-old man from Moldova, living in the Czech Republic, who had worked as a locksmith on oil platforms in Turkmenistan, Kazakhstan, Sudan, and Iraq since 1999, and was admitted to a neurology ward for a sudden motion disorder of the right leg, dysarthria, and hypomimia. Imaging revealed presence of expansive focus around the left lateral ventricle of the brain and a pronounced peripheral edema. The intracranial infectious focus was excised under intraoperative SonoWand guidance. Tissue samples were histologically positive for dark-pigmented hyphae, suggesting dematiaceous fungi. Therefore, liposomal amphotericin B therapy was initiated immediately. Fonsecaea monophora was provisionally identified using ITS rDNA region sequencing directly from brain tissue. The identification was subsequently confirmed by cultivation and DNA sequencing from culture. The strain exhibited in vitro sensitive to voriconazole (MIC = 0.016 μg/mL) and resistance to amphotericin B (MIC = 4 μg/mL); therefore, the amphotericin B was replaced with voriconazole. Postoperatively, a significant clinical improvement was observed and no additional surgery was required. Based on the literature review, this is the third documented case of cerebral infection due to this pathogen in patients without underlying conditions and the first such case in Europe.


Similar content being viewed by others
References
Bagla P, Loeffelholz M, Blanton LS (2016) Cerebral phaeohyphomycosis by Fonsecaea monophora: report in a patient with AIDS and a ring enhancing lesion. Med Mycol Case Rep 12:4–7. https://doi.org/10.1016/j.mmcr.2016.06.002
Chowdhary A, Meis JF, Guarro J, de Hoog GS, Kathuria S, Arendrup MC, Arikan-Akdagli S, Akova M, Boekhout T, Caira M, Guinea J, Chakrabarti A, Dannaoui E, van Diepeningen A, Freiberger T, Groll AH, Hope WW, Johnson E, Lackner M, Lagrou K, Lanternier F, Lass-Flörl C, Lortholary O, Meletiadis J, Muñoz P, Pagano L, Petrikkos G, Richardson MD, Roilides E, Skiada A, Tortorano AM, Ullmann AJ, Verweij PE, Cornely OA, Cuenca-Estrella M, European Society of Clinical Microbiology and Infectious Diseases Fungal Infection Study Group, European Confederation of Medical Mycology (2014) ESCMID and ECMM joint clinical guidelines for the diagnosis and management of systemic phaeohyphomycosis: diseases caused by black fungi. Clin Microbiol Infect 20(Suppl 3):47–75. https://doi.org/10.1111/1469-0691.12515
De Hoog GS, Attili-Angelis D, Vicente VA, Van Den Ende AH, Queiroz-Telles F (2004) Molecular ecology and pathogenic potential of Fonsecaea species. Med Mycol 42:405–416
de Hoog GS, Nishikaku AS, Fernandez-Zeppenfeldt G, Padín-González C, Burger E, Badali H, Richard-Yegres N, van den Ende AHGG (2007) Molecular analysis and pathogenicity of the Cladophialophora carrionii complex, with the description of a novel species. Stud Mycol 58:219–234. https://doi.org/10.3114/sim.2007.58.08
Doymaz MZ, Seyithanoglu MF, Hakyemez I, Gultepe BS, Cevik S, Aslan T (2015) A case of cerebral phaeohyphomycosis caused by Fonsecaea monophora, a neurotropic dematiaceous fungus, and a review of the literature. Mycoses 58:187–192. https://doi.org/10.1111/myc.12290
Goralska K, Blaszkowska J, Dzikowiec M (2018) Neuroinfections caused by fungi. Infection 46:443–459. https://doi.org/10.1007/s15010-018-1152-2
Koo S, Klompas M, Marty FM (2010) Fonsecaea monophora cerebral phaeohyphomycosis: case report of successful surgical excision and voriconazole treatment and review. Med Mycol 48:769–774. https://doi.org/10.3109/13693780903471081
Lucasse C, Chardome J, Magis P (1954) Cerebral mycosis from Cladosporium trichoides in a native of the Belgian Congo. Annales de la Societe Belge de Medecine Tropicale (1920) 34:475–478
Maertens JA, Raad II, Marr KA, Patterson TF, Kontoyiannis DP, Cornely OA, Bow EJ, Rahav G, Neofytos D, Aoun M, Baddley JW, Giladi M, Heinz WJ, Herbrecht R, Hope W, Karthaus M, Lee DG, Lortholary O, Morrison VA, Oren I, Selleslag D, Shoham S, Thompson GR III, Lee M, Maher RM, Schmitt-Hoffmann AH, Zeiher B, Ullmann AJ (2016) Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by aspergillus and other filamentous fungi (SECURE): a phase 3, randomised-controlled, non-inferiority trial. Lancet 387:760–769. https://doi.org/10.1016/s0140-6736(15)01159-9
Najafzadeh MJ, Sun J, Vicente VA, Klaassen CHW, Bonifaz A, van den Ende AHGG, Menken SBJ, Sybren de Hoog G (2011) Molecular epidemiology of Fonsecaea species. Emerg Infect Dis 17:464–469. https://doi.org/10.3201/eid1703.100555
Nobrega JP, Rosemberg S, Adami AM et al (2003) Fonsecaea pedrosoi cerebral phaeohyphomycosis (“chromoblastomycosis”): first human culture-proven case reported in Brazil. Rev Inst Med Trop Sao Paulo 45:217–220
Queiroz-Telles F, de Hoog S, Santos DWC et al (2017) Chromoblastomycosis. Clin Microbiol Rev 30:233–276
Schwartz S, Reisman A, Troke PF (2011) The efficacy of voriconazole in the treatment of 192 fungal central nervous system infections: a retrospective analysis. Infection 39:201–210. https://doi.org/10.1007/s15010-011-0108-6
Stokes W, Fuller J, Meier-Stephenson V, Remington L, Meatherall BL (2017) Case report of cerebral phaeohyphomycosis caused by Fonsecaea monophora. Off J Assoc Med Microbiol Infect Dis Canada 2:86–92
Surash S, Tyagi A, De Hoog GS et al (2005) Cerebral phaeohyphomycosis caused by Fonsecaea monophora. Med Mycol 43:465–472
Takei H, Goodman JC, Powell SZ (2007) Cerebral phaeohyphomycosis caused by Cladophialophora bantiana and Fonsecaea monophora: report of three cases. Clin Neuropathol 26:21–27
Varghese P, Jalal MJA, Ahmad S, Khan Z, Johny M, Mahadevan P, Joseph L, Chandy R, Paul S (2016) Cerebral Phaeohyphomycosis caused by Fonsecaea monophora: first report from India. Int J Surg Med 2:44–49
Zhang J, Wang L, Xi L, Huang H, Hu Y, Li X, Huang X, Lu S, Sun J (2013) Melanin in a meristematic mutant of Fonsecaea monophora inhibits the production of nitric oxide and Th1 cytokines of murine macrophages. Mycopathologia 175:515–522. https://doi.org/10.1007/s11046-012-9588-x
Acknowledgements
The contribution of VH was supported by the project BIOCEV (CZ.1.05/1.1.00/02.0109) provided by the Ministry of Education, Youth and Sports of CR and ERDF and Charles University Research Centre program No. 204069.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dobias, R., Filip, M., Vragova, K. et al. Successful surgical excision of cerebral abscess caused by Fonsecaea monophora in an immunocompetent patient and review of literature. Folia Microbiol 64, 383–388 (2019). https://doi.org/10.1007/s12223-018-0661-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12223-018-0661-9