2. Results and Discussion
In this synthetic procedure (
Scheme 1), several reaction steps were found requiring use of other approaches than originally planned ones. Either different reagents for successful completion of the target molecules had to be used or different approaches had to be selected. A selection of the reagents was often based on analogous synthetic procedures done earlier during our projects focused on steroids and triterpenoid acids [
10]. Therefore, a more detailed investigation and/or optimization in the synthesis of
8 and
6 was made. We mostly focused on a behavior of the source molecules (
7 and
5) during the synthesis, in which several procedures, earlier developed in our team, were used in the synthesis of triterpenoid acid derivatives, and in analogous reactions [
10,
11,
12,
13,
14,
15,
16]. A hypothesis on the course of the palladium-catalyzed hydrogenation in its employed modifications is postulated.
The first step of the synthetic procedure (
Scheme 1) consisted in a conversion of the carboxyl group in
2 into its benzyl ester
3 by reacting
2 with benzyl bromide in DMF, under the presence of potassium carbonate [
11,
17]. Subsequently, the C(3)-OH group of
3 was converted into the corresponding propargyl ether
4 using propargyl bromide, in the presence of sodium hydride in THF [
18]. Note that it is important to mix
3 with sodium hydride at least 30 min before adding propargyl bromide, to enable a formation of the sodium salt of
3. The originally used methods of etherification, employing either propargyl chloride [
18] or propargylic alcohol in chloroform under the presence of Montmorillonit K [
19], were not successful in this case. The propargyl ether
4 was subjected to a click reaction (Huisgen copper(I)-catalyzed 1,3-dipolar cycloaddition, CuAAC) with azidovaleric acid under a catalysis with copper(II) sulfate in a water-dichloromethane mixture, yielding
5. TBTA was used as stabilizer of the Cu(I) oxidation state in aqueous solutions as well as acted as a rate-accelerating ligand [
20,
21]. To stabilize Cu(I) oxidation state is important because Cu(II) ions are harmful to this reaction due to the fact that Cu(II) ions catalyze the oxidative coupling of the alkyne substrates to give diynes as undesired by-products [
20]. Sodium ascorbate acts as a reducing agent.
The main quantity of
5 was used for modification of the diosgenin molecule (
1) by Steglich esterification with
5 under the presence of
N,
N’-dicyclohexylcarbodiimide (DCC) as coupling agent, and 4-(dimethylamino)pyridine (DMAP) as reaction enhancer, to get
7. This reaction is an example of esterification that was not mediated successfully with 1-propanephosphonic anhydride (T3P), another coupling agent. T3P had often been used for formation of ester or amide bonds in our team [
11]. Generally, we prefer using T3P over DCC since phosphonic acid products resulting from the T3P hydrolysis are soluble in water and are not extracted with organic solvents in contrast to dicyclohexyl urea resulting from DCC. We also tried to convert
5 to its acyl chloride with oxalyl chloride; however, this method did not yield the required product. Finally, the resulting product
7 was subjected to a high-pressure (130 kPa) hydrogenation on 10% Pd/C in an ethanol-THF mixture, yielding the target diosgenin conjugate
8.
A deprotection of
5 and
7 was carried out in a different way than customary used procedure [
10] in our laboratory (entry 1,
Table 1) due to its failure. This result inspired us to search for other methods of deprotection of
5 and
7. First, we have employed hydrogenation under atmospheric pressure (entries 2, 3 and 4 [
22]) to obtain
8. However, the hydrogenation has not been catalyzed quantitatively. Using BCl
3 in dichloromethane (entry 5 [
23]) showed no reaction, and using HBr in acetic acid (entry 6 [
24]) resulted in a decomposition of the starting material. Originally, the main reason for employing hydrogenation reaction under atmospheric pressure was to prevent possible saturation of the C(20)=C(29) double bond in the betulinic acid unit of
6 and
8. When this reaction did not furnish
6 and
8, we have investigated hydrogenation under slightly higher pressure than atmospheric pressure, using a different palladium catalyst (entry 7). Nevertheless, it also did not catalyze the reaction in the required way. Finally, the high pressure hydrogenation procedure [
17] was the successful method for deprotection of
5 and
7 and it occurred without saturating the C(20)=C(29) double bond (entries 8 and 10). However, when the pressure increased the value of 130 kPa (entry 9), saturation of the double bond appeared, indicating that 130 kPa is the critical pressure to keep the C(20)=C(29) double bond in
8 unsaturated. Saturation of the C(20)=C(29) double bond was proven by the presence of a peak belonging to the saturated product in the HR-MS spectra. Saturated product was isolated from the TLC plate and dissolved in methanol prior to measurement. It was an unexpected result, because transferring hydrogenation under atmospheric pressure was used successfully for removal of protecting benzyl group from carboxylic benzyl esters several times [
10,
11,
13]. The reason for the failing of transferring hydrogenation in the removal of the benzyl group from
5 and
7 to get
6 and
8 can be explained by a simultaneous presence of the 1,4-disubstituted 1,2,3-triazole ring in the molecule, a phenomenon that had already been observed earlier in the literature [
25]. The 1,4-disubstituted 1,2,3-triazole ring probably shows its competing effect in coordination of palladium catalyst over the target site, requiring a different approach than usually used for the successful course of the debenzylation reaction. See also
Scheme S1 in the Supplementary Material.
Removal of the benzyl protecting group from
5 using the above described high pressure (130 kPa) hydrogenation was also made to prepare
6, the other target product for pharmacological screening. HR-MS ESI supported successful removal of the benzyl protecting group of
7, while keeping the C(20)=C(29) double bond unsaturated. In HR-MS ESI of
6 and
8, typical adducts [M − H]
− were observed, C
38H
59O
5N
3 (for
6), or C
65H
99O
7N
3 (for
8), respectively. In HR-MS of
4,
5, and
7, adducts [M − H]
+ were identified (
Table 2).
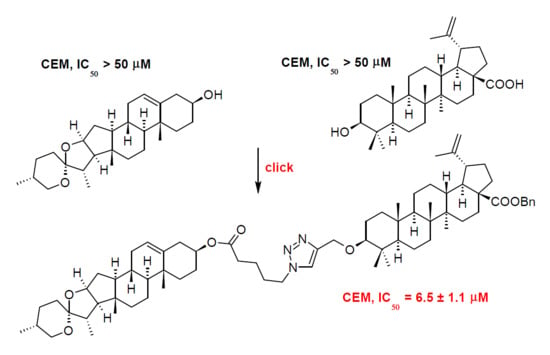
The compounds
1–
8 were subjected to the cytotoxicity screening tests on cells of human T-lymphoblastic leukemia (CEM), cells of human breast adenocarcinoma (MCF7), cells of human cervical cancer (HeLa), and human colon carcinoma (HCT 116 cancer cell lines), using normal human fibroblasts (BJ) as reference cell lines. Doxorubicin was used as a positive control. While the target compounds
6 and
8 were inactive, due to a possible high polarity, causing a decrease in ability of the studied compounds to penetrate into the cell,
5 showed moderate to weak multifarious cytotoxicity to all cancer cell lines. Benzyl ester of the main target compound (
7) displayed a selective cytotoxicity on CEM (6.5 ± 1.1 µM), but also weak cytotoxicity (46.2 ± 2.8 µM) towards the reference cell line BJ (
Table 3).
To support the data obtained experimentally, physico-chemical and ADME parameters of the synthesized compounds have been calculated using ACD/iLabs software and databases [
27] for
1–
8 (
Table 4). The data were compared with the Lipinski rule of five [
28] and with the Ghose [
29] rule. The Lipinski [
28] and Ghose [
29] rules were postulated for testing in vivo. Nevertheless, they are applicable in the screening tests in cancer cell lines, as we have proven several times in our previous papers [
13,
14,
15]. However, deviations of experimental and calculated values have already been observed [
16]. The rules describe molecular properties important for a small molecule drug pharmacokinetics in the human body, including their absorption, distribution, metabolism, and excretion (known as ADME parameters). However, the rules do not predict displaying of the pharmacological activity. The Lipinski rule of five [
28] and Ghose rule [
29] consider partition coefficient (log
P, range −0.4 to +5.6), molar refractivity (range 40 to 130), molecular weight (range 180 to 500), number of atoms in the molecule (20 to 70), and polar surface area (up to 14 nm). However, the parameters calculated for some of the target compounds
1–
8 correspond only in part to the ranges given for them by the above Lipinski [
28] and Ghose [
29] rules (
Table 4). Despite those facts,
5 and
7, the only cytotoxic compounds of this series, displayed cytotoxicity. For more details on calculation, explanation, and importance of physico-chemical and ADME characteristics in searching for novel potential drugs cf.
Supplementary Materials.
Calculated activity on central nervous system (CNS) for
1 and
2 resulted in a finding that
1 is CNS active, while
2 appears in the area with low or no CNS activity, also made by the ACD/iLabs software [
27]. The data obtained show the key parameters for assigning CNS activity, log
PS*
fu, brain (the brain/plasma equilibration rate), log
BB (a hybrid parameter determined by permeability, plasma and brain tissue binding and active transport mechanism; range +1.2 to −3.0), and log
PB (the extent of brain penetration parameter, indicating if the drug might be CNS active or CNS inactive; range +2 (CNS active) to −2 (CNS inactive); cf.
Table 4 and
Figure S1 in the Supplementary Material). Based on the values of log
PS*
fu,brain, log
PB and log
BB (
Table 4),
1 when liberated from
7 or
8 by their metabolic decomposition, may display certain activity on central nervous system, which may result in additional positive adaptogenic effect on organism if applied in vivo.
3. Material and Methods
3.1. General
The NMR measurements were performed either on a Bruker AVANCE 500 MHz or on a Bruker AVANCE II 600 MHz spectrometer equipped with a 5 mm TCI cryoprobe in a 5 mm tube in different solvents. The
1H NMR and the
13C NMR spectra were recorded at 499.98 MHz and 125.73 MHz (AVANCE 500 MHz) or at 600.13 MHz and 150.90 MHz (AVANCE II 600 MHz) in CDCl
3 or CD
3OD using tetramethylsilane (δ = 0.0 − CDCl
3) or signal of solvent (δ = 3.31 or 49.50 for
1H/
13C − CD
3OD) as internal references.
1H NMR data are presented in the following order: chemical shift (δ) expressed in ppm, multiplicity (s, singlet; d, doublet; t, triplet; q, quartet; m, multiplet), number of protons, coupling constants in Hertz. For unambiguous assignment of both
1H and
13C signals, 2D NMR
1H,
13C gHSQC and gHMBC spectra were measured using standard parameters sets and pulse programs delivered by producer of the spectrometer. Infrared spectra were measured with a Nicolet 205 FT-IR spectrometer (Thermofisher Scientific, Waltham, MA, USA). HR-MS was acquired on Exactive Plus Orbitrap Mass Spectrometer with HESI (coin voltage 4.5 kV, resolution 100,000 @ 1 Hz, capillary temperature 300 °C, probe temperature 30−40 °C) and were processed in Xcalibur™ 2.1 SW (ThermoFisher Scientific, Waltham, MA, USA). Samples were dissolved in methanol. See
Supplementary Material for more details on HR-MS (ESI) analyses (
Table 1). TLC was carried out on silica gel plates (Merck 60F
254, Merck, Prague, Czech Republic) and the visualization was performed by both the UV detection and spraying with the methanolic solution of phosphomolybdic acid (5%) followed by heating. For column chromatography, silica gel 60 (0.063–0.200 mm) from Merck was used. All chemicals and solvents were purchased from regular commercial sources in analytical grade and the solvents were purified by general methods before use. Betulinic acid was purchased from Dr. Jan Šarek—Betulinines (
www.betulinines.com). Diosgenin was purchased from Wako Chemicals (Osaka, Japan). Analytical HPLC was carried out on a TSP (Thermoseparation Products, Boston, MA, USA) instrument equipped with a ConstaMetric 4100 Bio pump and a SpectroMonitor 5000 UV DAD. The analyses of the products were performed on a reverse phase Nucleosil 120-5 C18 column (250 × 4 mm; Watrex, Prague, Czech Republic) using a methanol/water mixture (9:1,
v/
v) as mobile phase at 0.5 to 1.0 mL.min
−1. The eluate was monitored at 220, 254, and 275 nm, and the UV spectra were run from 200 to 300 nm.
3.2. Benzyl (3β)-3-hydroxylup-20(29)-en-28-oate (3)
Benzyl bromide (0.65 mL; 5.48 mmol) was added to a solution of betulinic acid (2; 1.0 g; 2.19 mmol) in acetone (40 mL), in a presence of potassium carbonate (0.45 g; 3.28 mmol), and the reaction mixture was stirred at r.t. for 24 h. The mixture was worked-up by diluting it with chloroform and extracted with water. Organic layer was dried with sodium sulfate, then the solvent was evaporated under reduced pressure, and the residue was purified by chromatography using chloroform/EtOH mixture as mobile phase yielding 3 as white powder in a 99% yield (1.19 g). 1H-NMR (499.98 MHz, CDCl3): δ [ppm] 0.61 (dd, 1H, J = 2.5; 11.3 Hz, H-5), 0.70 (s, 3H, H-23), 0.71 (s, 3H, H-24), 0.75 (d, 3H, J = 0.7 Hz, H-25), 0.90 (d, 3H, J = 0.6 Hz, H-26), 0.91 (s, 3H, H-27), 1.05 (dt, 2H, J = 3.0; 3.0; 13.2 Hz, H-21), 1.63 (dd, 3H, J = 0.7; 1.4 Hz, H-30), 2.14 (ddd, 1H, J = 3.7; 11.6; 12.9 Hz, H-13), 2.23 (dt, 2H, J = 3.4; 3.4; 12.5 Hz, H-16), 2.97 (dt, 1H, J = 4.6; 11.0; 11.0 Hz, H-19), 3.13 (dd, 1H, J = 4.9; 11.4 Hz, H-3), 4.55 (dq, 2H, J = 1.4; 1.4; 1.4; 2.4 Hz, H-29), 4.68 (dq, 2H, J = 0.7; 0.7; 0.7; 2.4 Hz, H-29), 5.05 (d, 2H, J = 12.3 Hz, H-1′), 5.10 (d, 2H, J = 12.3 Hz, H-1′), 7.24–7.35 (m, 2H, H-3′,H-4′,H-5′). 13C-NMR (125.73 MHz, CDCl3): δ [ppm] 14.66 (q, C-27), 15.34 (q, C-24), 15.81 (q, C-25), 16.11 (q, C-26), 18.27 (t, C-6), 19.35 (q, C-29), 20.85 (t, C-11), 25.51 (t, C-12), 27.39 (t, C-2), 27.96 (q, C-23), 29.55 (t, C-21), 30.56 (t, C-15), 32.10 (t, C-16), 34.28 (t, C-22), 36.92 (t, C-7), 37.15 (s, C-10), 38.18 (d, C-13), 38.69 (t, C-1), 38.83 (s, C-4), 40.62 (s, C-8), 42.37 (s, C-14), 46.91 (d, C-19), 49.42 (d, C-18), 50.53 (d, C-9), 55.32 (d, C-5), 56.53 (s, C-17), 65.71 (t, C-1′), 78.96 (d, C-3), 109.56 (t, C-30), 128.04 (d, C-5′), 128.22 (d, C-4′), 128.47 (d, C-3′), 136.47 (s, C-2′), 150.57 (s, C-20), 175.80 (s, C-28). IR (KBr): [cm−1] 3533 s (O-H) stretching, 2940 s (ring system, sp3, C-H) stretching, 1692 s (C=O) stretching, 1647 w (benzene, C=C) stretching, 1453 m (benzene, C=C) stretching, 1184, 757, 699. HR-MS (ESI) m/z 547.4172, calcd. 547.4146 for C37H55O3.
3.3. Benzyl (3β)-3-(prop-2-yn-1-yloxy)lup-20(29)-en-28-oate (4)
A portion of sodium hydride (0.48 g; 20.44 mmol) was added to a solution of 3 (0.325 g; 0.60 mmol) in THF (15 mL), and the mixture was stirred at r.t. for 30 min. Then, an additional portion of sodium hydride (0.48 g; 20.44 mmol) was added, and the mixture was stirred for an additional 30 min. Propargyl bromide (0.176 mL; 2.32 mmol) was added, and the mixture was stirred at r.t. for 24 h. Then, additional propargyl bromide (0.137 mL; 1.80 mmol) was added, and the mixture was stirred at r.t. for an additional 24 h. The reaction was then worked-up by extraction with chloroform (4 × 15 mL). The extract was washed with water, dried over sodium sulfate, filtered, and the solvent was evaporated under reduced pressure. The residue was purified by column chromatography on silica gel, using petroleum ether/chloroform as mobile phase, yielding 4 in a 96% (0.336 g) yield. 1H-NMR (499.98 MHz, CDCl3): δ [ppm] 0.61 (dd, 1H, J = 2.2; 11.3 Hz, H-5), 0.68 (s, 3H, H-23), 0.69 (s, 3H, H-24), 0.73 (s, 3H, H-25), 0.87 (d, 3H, J = 0.6 Hz, H-26), 0.89 (s, 3H, H-27), 1.02 (dt, 2H, J = 3.2; 3.2; 13.1 Hz, H-21), 1.61 (dd, 3H, J = 0.7; 1.4 Hz, H-30), 2.11 (ddd, 1H, J = 3.7; 11.5; 12.9 Hz, H-13), 2.21 (dt, 2H, J = 2.9; 2.9; 12.3 Hz, H-16), 2.29 (t, 1H, J = 2.4 Hz, H-3′), 2.92 (dd, 1H, J = 4.4; 11.8 Hz, H-3), 2.95 (dt, 1H, J = 5.8; 11.2; 11.2 Hz, H-19), 4.07 (dd, 2H, J = 2.4; 16.0 Hz, H-1′), 4.15 (dd, 2H, J = 2.4; 16.0 Hz, H-1′), 4.52 (dq, 2H, J = 1.4; 1.4; 1.4; 2.4 Hz, H-29), 4.66 (dq, 2H, J = 0.7; 0.7; 0.7; 2.4 Hz, H-29), 5.02 (d, 2H, J = 12.3 Hz, H-4′), 5.07 (d, 2H, J = 12.3 Hz, 4′), 7.23–7.32 (m, 2H, H-6′, H-7′, H-8′). 13C-NMR (125.73 MHz, CDCl3): δ [ppm] 14.62 (q, C-27), 15.82 (q, C-24), 16.10 (q, C-25), 16.17 (q, C-26), 18.21 (t, C-6), 19.37 (q, C-29), 20.89 (t, C-11), 25.54 (t, C-12), 27.96 (t, C-2), 29.54 (q, C-23), 30.17 (t, C-21), 30.57 (t, C-15), 32.10 (t, C-16), 34.29 (t, C-22), 36.93 (t, C-7), 37.11 (t, C-10), 38.18 (d, C-13), 38.53 (t, C-1), 38.56 (s, C-4), 40.67 (s, C-8), 42.37 (s, C-14), 46.92 (d, C-19), 49.44 (d, C-18), 50.52 (d, C-9), 55.89 (d, C-5), 56.38 (t, C-1′), 56.53 (s, C-17), 65.71 (t, C-4′), 73.39 (d, C-3), 80.83 (d, C-3′), 80.95 (s, C-2′), 109.55 (t, C-30), 128.04 (d, C-8′), 128.23 (d, C-7′), 128.47 (d, C-6′), 136.47 (s, C-5′), 150.60 (s, C-20), 175.79 (s, C-28). IR (KBr): [cm−1] 3305 m (sp, C-H) stretching, 2957 s (ring system, sp3, C-H) stretching, 1715 s (C=O), 1644 w (benzene, C=C) stretching, 1453 m (benzene, C=C), 1128, 1080, 755, 628. HR-MS (ESI) m/z 585.4289, calcd. 585.4302 for C40H57O3.
3.4. 5-[4-({[(3β)-28-(Benzyloxy)-28-oxolup-20(29)-en-3-yl]oxy}-methyl)-1H-1,2,3-triazol-1-yl]pentanoic acid (5)
5-Azidovaleric acid (61.27 mg; 0.43 mmol), sodium ascorbate (16.94 mg; 0.09 mmol) and a solution of CuSO4·5H2O with TBTA in water (7.61 mL; 0.89 mmol) was added to a solution of 4 (200 mg; 0.34 mmol) in CH2Cl2 (5 mL), and the mixture was stirred at r.t. for 30 h. The mixture was worked-up by extraction with methylene chloride, the extract was washed with water, and dried over sodium sulfate. After filtration, the solvent was evaporated under reduced pressure, and the residue was purified by column chromatography on silica gel, using petroleum ether/chloroform mixture as mobile phase, yielding 5 in a 95% yield (0.26 g). 1H-NMR (499.98 MHz, CDCl3): δ [ppm] 0.58 (dd, 1H, J = 2.3; 11.2 Hz, H-5), 0.68 (s, 3H, H-23), 0.68 (s, 3H, H-24), 0.73 (s, 3H, H-25), 0.81 (s, 3H, H-26), 0.86 (s, 3H, H-27), 1.02 (dt, 2H, J = 3.2; 3.2; 13.5 Hz, H-21), 1.52 (t, 1H, J = 11.4 Hz, H-18), 1.53–1.65 (m, 2H, H-5′, H-6′), 1.61 (dd, 3H, J = 0.7; 1.4 Hz, H-30), 2.10 (ddd, 1H, J = 3.6; 11.5; 12.8 Hz, H-13), 2.20 (dt, 2H, J = 3.1; 3.1; 12.5 Hz, H-16), 2.33 (t, 2H, J = 7.3 Hz, H-7′), 2.87 (dd, 1H, J = 4.4; 11.8 Hz, H-3), 2.95 (dt, 1H, J = 4.8; 11.0; 11.0 Hz, H-19), 4.30 (t, 2H, J = 7.1 Hz, H-4′), 4.49 (dd, 2H, J = 0.6; 12.5 Hz, H-1′), 4.53 (dq, 2H, J = 1.4; 1.4; 1.4; 2.4 Hz, H-29), 4.65 (dq, 2H, J = 0.7; 0.7; 0.7; 2.4 Hz, H-29), 4.70 (dd, 2H, J = 0.6; 1.2 Hz, H-1′), 5.02 (d, 2H, J = 12.3 Hz, H-9′), 5.07 (d, 2H, J = 12.3 Hz, H-9′), 7.22–7.32 (m, 2H, H-11′, H-13′), 7.44 (s, 1H, H-3′). 13C-NMR (125.73 MHz, CDCl3): δ [ppm] 14.61 (q, C-27), 15.81 (q, C-24), 16.12 (q, C-25), 16.25 (q, C-26), 18.20 (t, C-6), 19.34 (q, C-29), 20.87 (t, C-11), 21.52 (t, C-6′), 22.89 (t, C-5′), 25.51 (t, C-12), 27.99 (q, C-23), 28.19 (t, C-2), 29.51 (t, C-15), 30.55 (t, C-21), 32.09 (t, C-16), 32.97 (t, C-7′), 34.26 (t, C-22), 36.92 (t, C-7), 37.11 (s, C-10), 38.17 (d, C-13), 38.50 (t, C-1), 38.78 (s, C-4), 40.65 (s, C-8), 42.35 (s, C-14), 46.92 (d, C-19), 49.42 (d, C-18), 49.85 (t, C-4′), 50.47 (d, C-9), 55.70 (d, C-5), 56.53 (s, C-17), 63.18 (t, C-1′), 65.70 (t, C-9′), 86.61 (d, C-3), 109.57 (t, C-30), 122.09 (d, C-3′), 128.02 (d, C-13′), 128.21 (d, C-12′), 128.46 (d, C-11′), 136.46 (s, C-10′), 146.55 (s, C-2′), 150.56 (s, C-20), 175.81 (s, C-28), 177.46 (s, C-8′). IR (KBr): [cm−1] 2945 s br (ring system, sp3 C-H and O-H overlap) stretching, 1732 s (C=O) stretching, 1642 w (benzene, C=C) stretching, 1453 m (benzene, C=C) stretching, 1130. HR-MS (ESI) m/z 728.4987, calcd. 728.4997 for C45H66O5N3.
3.5. (3β)-3-{[1-(4-Carboxybutyl)-1H-1,2,3-triazol-4-yl]methoxy}lup-20(29)-en-28-oic Acid (6)
The compound 5 (75 mg, 0.105 mmol) was subjected to a removal of the benzyl protecting group by hydrogenation on a 10% Pd/C (75 mg, 0.705 mmol) in a THF/ethanol (1:1) mixture (8 mL) at 130 kPa at r.t. for 30 min. After filtering the mixture off to remove the catalyst, and evaporation of the solvent, the residue was purified by column chromatography, using petroleum ether/ethyl acetate as mobile phase, yielding 6 in a 92% yield (61.3 mg). 1H-NMR (600.13 MHz, CDCl3): δ [ppm] 0.61 (dd, 1H, J = 1.9; 11.4 Hz, H-5), 0.68 (s, 3H, H-25), 0.75 (s, 3H, H-24), 0.81 (d, 3H, J = 0.6 Hz, H-23), 0.84 (d, 3H, J = 0.8 Hz, H-26), 0.89 (d, 3H, J = 0.5 Hz, H-27), 1.54 (t, 1H, J = 11.4 Hz, H-18), 1.58 (dd, 3H, J = 0.7; 1.4 Hz, H-30), 2.09 (ddd, 1H, J = 3.8; 11.8; 12.8 Hz, H-13), 2.19 (ddd, 2H, J = 3.2; 3.7; 13.1 Hz, H-16), 2.34 (t, 2H, J = 7.2 Hz, H-7′), 2.89 (dd, 1H, J = 4.4; 11.7 Hz, H-3), 2.92 (dt, 1H, J = 4.9; 11.0; 11.5 Hz, H-19), 4.31 (dt, 2H, J = 1.0; 7.0; 7.0 Hz, H-4′), 4.48 (dd, 2H, J = 0.7; 12.5 Hz, H-1′), 4.54 (dq, 2H, J = 1.4; 1.4; 1.4; 2.4 Hz, H-29), 4.67 (dq, 2H, J = 0.7; 0.7; 0.7; 2.4 Hz, H-29), 4.72 (dd, 2H, J = 0.6; 12.5 Hz, H-1′), 7.46 (s, 1H, H-3′). 13C-NMR (150.91 MHz, CDCl3): δ [ppm] 14.63 (q, C-27), 16.10 (q, C-24), 16.13 (q, C-26), 16.24 (q, C-25), 18.21 (t, C-6), 19.36 (q, C-29), 20.84 (t, C-6′), 21.51 (t, C-11), 22.93 (t, C-5′), 25.45 (t, C-12), 28.01 (q, C-23), 29.52 (t, C-2), 29.68 (t, C-15), 30.56 (t, C-21), 32.13 (t, C-16), 33.14 (t, C-7′), 34.25 (t, C-22), 37.05 (t, C-7), 37.14 (s, C-10), 38.40 (d, C-13), 38.50 (t, C-1), 38.80 (s, C-4), 40.67 (s, C-8), 42.38 (s, C-14), 46.90 (t, C-19), 49.28 (d, C-18), 49.91 (t, C-4′), 50.38 (d, C-9), 55.70 (d, C-5), 56.42 (s, C-17), 63.31 (t, C-1′), 86.73 (d, C-3), 109.69 (t, C-30), 122.10 (d, C-3′), 146.60 (s, C-2′), 150.39 (s, C-20), 178.37 (s, C-28), 182.46 (s, C-8′). IR (KBr): [cm−1] 2944 s, (ring system, sp3 C-H and O-H overlap) stretching, 1705 s (C=O) stretching. HR-MS (ESI) m/z 636.4413, calcd. 636.4382 for C38H59O5N3.
3.6. Benzyl (3β)-3-[(1-{5-oxo-5-[(3β,25R)-spirost-5-en-3-yloxy]pentyl}-1H-1,2,3-triazol-4-yl)methoxy]lup-20(29)-en-28-oate (7)
DCC (167.0 mg, 0.81 mmol) and DMAP (152.5 mg, 1.25 mmol) were added to a solution of 5 (168 mg, 0.23 mmol) in methylene chloride (10 mL) under stirring. Then, diosgenin (1; 143 mg, 0.35 mmol) was added, and stirring continued at r.t. for 24 h. The crude product was purified by column chromatography on silica gel using petroleum ether/ethyl acetate as mobile phase, yielding white, crystalline 7 in a 72% yield (186 mg). 1H-NMR (600.13 MHz, CDCl3): δ [ppm] 0.64 (dd, 1H, J = 2.1; 11.2 Hz, H-5), 0.74 (s, 3H, H-23), 0.74 (s, 3H, H-19″), 0.76 (s, 3H, H-25), 0.78 (d, 3H, H-27″), 0.86 (s, 3H, H-24), 0.92 (s, 3H, H-26), 0.96 (d, 3H, J = 7.0 Hz, H-21″), 1.02 (s, 3H, H-27), 1.02 (s, 3H, H-18″), 1.67 (dd, 3H, J = 0.7; 1.4 Hz, H-30), 2.16 (ddd, 1H, J = 3.5; 11.6; 12.8 Hz, H-13), 2.26 (dt, 2H, J = 3.1; 3.1; 12.7 Hz, H-16), 2.31 (t, 2H, J = 7.3 Hz, H-12′), 2.93 (dd, 1H, J = 4.3; 11.7 Hz, H-3), 3.01 (dt, 1H, J = 4.9; 10.9; 10.9 Hz, H-19), 3.37 (t, 2H, J = 11.0 Hz, H-26″), 3.44–3.50 (m, 2H, H-26″), 3.44–3.50 (m, 1H, H-20″), 4.35 (t, 2H, J = 7.0 Hz, H-9′), 4.40 (ddd, 1H, J = 6.5; 7.6; 8.5 Hz, H-16″), 4.54 (dd, 2H, J = 0.5; 12.5 Hz, H-6′), 4.58 (dq, 2H, J = 1.4; 1.4; 1.4; 2.3 Hz, H-29), 4.59 (dddd, 2H, J = 4.3; 6.5; 10.6; 11.4 Hz, H-3″), 4.71 (dq, 2H, J = 0.7; 0.7; 0.7; 2.3 Hz, H-29), 4.76 (dd, 2H, J = 0.5; 12.5 Hz, H-6′), 5.08 (dd, 2H, J = 0.5; 12.5 Hz, H-1′), 5.13 (dd, 2H, J = 0.5; 12.5 Hz, H-1′), 5.36 (dt, 2H, J = 0.9; 0.9; 5.3 Hz, H-6″), 7.28–7.37 (m, 2H, H-3′-H-5′). 13C-NMR (150.91 MHz, CDCl3): δ [ppm] 14.51 (q, C-21″), 14.62 (q, C-27), 16.12 (q, C-25), 16.25 (q, C-18″), 16.26 (q, C-24), 17.12 (q, C-27″), 18.22 (t, C-6), 19.32 (q, C-29), 19.34 (q, C-19″), 20.77 (t, C-11″), 20.87 (t, C-11), 21.84 (t, C-10′), 22.89 (t, C-11′), 23.82 (t, C-2), 25.51 (t, C-12), 25.82 (q, C-26), 27.74 (q, C-23), 28.78 (t, C-24″), 29.53 (t, C-21), 29.62 (t, C-23″), 30.28 (d, C-8″), 30.56 (t, C-15), 31.37 (t, C-2″), 31.37 (d, C-25″), 31.81 (t, C-7″), 32.02 (t, C-15″), 32.10 (t, C-16), 33.89 (t, C-12′), 33.89 (t, C-12″), 34.28 (t, C-22), 36.70 (s, C-10″), 36.91 (s, C-10), 36.93 (t, C-7), 37.12 (t, C-1″), 38.08 (s, C-4), 38.18 (d, C-13), 38.51 (t, C-1), 40.66 (s, C-8), 40.83 (s, C-13″), 41.59 (t, C-4″), 42.36 (s, C-14), 46.93 (d, C-19), 49.21 (d, C-20″), 49.43 (d, C-18), 49.90 (t, C-9′), 49.91 (d, C-9″), 50.48 (d, C-9), 55.71 (d, C-5), 56.41 (d, C-14″), 56.53 (s, C-17), 62.05 (d, C-17″), 63.22 (t, C-6′), 65.70 (t, C-1′), 66.83 (t, C-26″), 74.01 (d, C-3″), 80.78 (d, C-16″), 86.49 (d, C-3), 109.27 (s, C-22″), 109.58 (t, C-30), 122.01 (d, C-8′), 122.44 (d, C-6″), 128.03 (d, C-5′), 128.22 (d, C-4′), 128.46 (d, C-3′), 136.47 (s, C-2′), 139.56 (s, C-5″), 146.55 (s, C-7′), 150.57 (s, C-20), 175.80 (s, C-28). IR (KBr): [cm−1] 2945 s, (ring system, sp3, C-H) stretching, 1731 s (C=O), 1626 m (alkene, C=C) stretching, 1456 m (benzene, C=C) stretching, 1128. HR-MS (ESI) m/z 1124.8025, calcd. 1124.8023 for C72H105O7N3.
3.7. (3β)-3-[(1-{5-Oxo-5-[(3β,25R)-spirost-5-en-3-yloxy]pentyl}-1H-1,2,3-triazol-4-yl]methoxy}lup-20(29)-en-28-oic Acid (8)
The benzyl ester 7 (186.3 mg, 0.166 mmol) was subjected to a hydrogenation on a 10% Pd/C (118.1 mg, 0.111 mmol) in a THF/ethanol (1:1; 10 mL) mixture at 130 kPa at r.t. for 40 min. The mixture was then filtered off and the product was purified by column chromatography on silica gel, using a chloroform/ethanol mixture (200:1) as mobile phase, yielding the product 8 in an 87% yield (149 mg). 1H-NMR (600.13 MHz, CDCl3): δ [ppm] 0.61 (dd, 1H, J = 1.9; 11.4 Hz, H-5), 0.69 (s, 3H, H-19′’), 0.72 (d, 3H, J = 6.4 Hz, H-27′’), 0.75 (s, 3H, H-18′’), 0.76 (s, 3H, H-25), 0.81 (s, 3H, H-23), 0.86 (s, 3H, H-24), 0.89 (s, 3H, H-26), 0.89 (s, 3H, H-27), 0.90 (d, 3H, J = 7.0 Hz, H-21′’), 0.96 (s, 3H, H-30), 2.12 (ddd, 1H, J = 3.8; 11.8; 12.8 Hz, H-13), 2.28 (ddd, 2H, J = 2.8; 4.6; 12.8 Hz, H-16), 2.88 (dd, 1H, J = 4.4; 11.7 Hz, H-3), 2.94 (dt, 1H, J = 5.0; 10.9; 10.9, H-19), 3.31 (t, 1H, J = 11.0 Hz, H-26′’), 3.41 (ddt, 1H, J = 1.8; 1.8; 5.0; 11.0 Hz, H-26′’), 4.34 (ddd, 1H, J = 6.4; 7.3; 8.5 Hz, H-16′’), 4.50 (d, 1H, J = 12.6 Hz, H-1′), 4.53 (dddd, 1H, J = 4.6; 6.3; 10.5; 11.7 Hz, H-3′’), 4.54 (dq, 1H, J = 3 × 1.4; 2.3 Hz, H-29), 4.67 (bd, 1H, J = 2.3 Hz, H-29), 4.70 (d, 1H, J = 12.6 Hz, H-1′), 5.30 (dt, 1H, J = 1.9; 1.9; 5.3 Hz, H-6′’), 7.45 (s, 1H, H-3′). 13C-NMR (150.91 MHz, CDCl3): δ [ppm] 14.48 (q, C-21′’), 14.65 (q, C-27), 16.08 (q, C-26), 16.17 (q, C-25), 16.27 (q, C-24), 16.27 (q, C-18′’), 17.12 (q, C-27′’), 18.23 (t, C-6), 19.33 (q, C-29), 19.36 (q, C-19′’), 20.81 (t, C-11′’), 20.87 (t, C-11), 21.83 (t, C-5′), 22.93 (t, C-2), 22.93 (t, C-6′), 25.47 (t, C-12), 28.03 (q, C-23), 28.77 (t, C-24′’), 29.35 (t, C-21), 29.56 (t, C-23′’), 30.27 (d, C-8′’), 30.56 (t, C-15), 31.36 (t, C-2′’), 31.36 (d, C-25′’), 31.80 (t, C-7′’), 32.01 (t, C-15′’), 32.17 (t, C-16), 33.68 (t, C-7′), 33.68 (t, C-12′’), 34.29 (t, C-22), 36.70 (s, C-10′’), 36.93 (s, C-10), 37.13 (t, C-7), 37.15 (t, C-1′’), 38.10 (s, C-4), 38.50 (d, C-13), 38.80 (t, C-1), 40.24 (s, C-8), 40.70 (s, C-13′’), 41.61 (t, C-4′’), 42.41 (s, C-14), 46.91 (d, C-19), 49.26 (d, C-20′’), 49.86 (d, C-18), 49.93 (t, C-4′), 49.93 (d, C-9′’), 50.42 (d, C-5), 55.70 (d, C-5), 56.25 (d, C-14′’), 56.42 (s, C-17), 62.00 (d, C-17′’), 63.26 (t, C-1′), 66.83 (t, C-26′’), 74.02 (d, C-3′’), 80.82 (d, C-16′’), 86.54 (d, C-3), 109.35 (s, C-22′’), 109.68 (t, C-30), 122.01 (d, C-3′), 122.45 (d, C-6′’), 139.56 (s, C-5′’), 146.64 (s, C-2′), 150.43 (s, C-20), 172.35 (s, C-8′), 179.92 (s, C-28). IR (KBr): [cm−1] 3322 m (O-H) stretching, 2928 s (ring system, sp3, C-H) streching, 1731 s (C=O) stretching, 1620 m (C=C) stretching → alkene, 1243, 1088. HR-MS (ESI) m/z 1033.7533, calcd. 1033.7483 for C65H99O7N3.
3.8. Cell Cultures
The screening cell lines, T-lymphoblastic leukemia (CEM), cervical carcinoma (HeLa), breast carcinoma (MCF7), and human foreskin fibroblasts (BJ) were obtained from the American Type Culture Collection (Manassas, VA, USA). Cells were cultured in DMEM (Dulbecco’s Modified Eagle Medium, Sigma Aldrich, Darmstadt, Germany). Media used were supplemented with 10% fetal bovine serum, 2 mM l-glutamine, and 1% penicillin-streptomycin (all from Sigma Aldrich, Darmstadt, Germany). The cell lines were maintained under standard cell culture conditions at 37 °C and 5% CO2 in humid environment. Cells were subcultured twice or three times a week using the standard trypsinization procedure.
3.9. Cytotoxicity Screening Tests
Description of the experimental procedure used in cytotoxicity assay was already published [
11]. The IC
50 values in CEM, MCF7, HeLa, HCT 116, and BJ measured with the compounds
1–
8 after 72 h of treatment are shown in
Table 3.